ATRIAL FIBRILLATION
This is an irregularity of the heartbeat, often very fast which can lead to clotting in the heart. It is associated with an increased risk of stroke and cardiac failure.
During an episode, the top parts of the heart (the atria) beat in a rapid and chaotic fashion; this is usually conducted rapidly to the bottom parts of the heart (the ventricles), which is why people experience a rapid heart rate. Some people with atrial fibrillation don’t experience any symptoms, and are unaware of their potential risk of stroke.
Sometimes atrial fibrillation occurs as an acute attack (paroxysmal) and other times the atrial fibrillation can be permanent. While the rhythm itself is not life threatening, urgent medical attention always needed to prevent the risk of stroke.
There are many treatments available for atrial fibrillation, the 2 main categories being medical treatment and catheter ablation. Appropriate anti-coagulation medications must also be considered to prevent the risk of stroke.
Common symptoms of atrial fibrillation include:
- Palpitations
- Chest discomfort
- Dizziness episodes
- Tiredness
- Decreased stamina
- Shortness of breath
- Fatigue
- Sometimes there are no symptoms
TYPES OF ATRIAL FIBRILLATION
Different types of atrial fibrillation, listing in order of increasing severity.
Paroxysmal atrial fibrillation. This type of atrial fibrillation comes and goes, and is usually associated with sudden onset of a fast heartbeat. It can occur at any age, but increases in incidence as we get older. Often a cardioversion is required, and sometimes medications or an ablation.
Persistent. This means that the heart is permanently in atrial fibrillation. This type is often more difficult to control, and a combined strategy of medications and or ablation is required.
Long-standing persistent. This means that the persistent atrial fibrillation lasts more than 12 months.
Permanent. This means that it is not possible to restore a normal heart rhythm. The atrium in these patients is often extensively diseased and scarred.
RISK FACTORS FOR ATRIAL FIBRILLATION
- Age. As we get older there is an increased risk of atrial fibrillation due to increased scarring (fibrosis) in the top chambers of our hearts.
- Valvar heart disease. Narrowing or leaking of any of the heart valves increases the risk of atrial fibrillation.
- Congenital heart disease. Patients with congenital heart disease have a marked increased incidence of atrial fibrillation
- Chronic health conditions. Chronic lung disease, kidney disease, diabetes all cause an increased risk of atrial fibrillation.
- High blood pressure. Poorly controlled high blood pressure increases the risk of atrial fibrillation
- Alcohol. Excess alcohol increases the risk of atrial fibrillation.
- Obesity. This increases the risk of atrial fibrillation.
- Family history. This puts some patients at an increased risk.
- Excessive exercise. While moderate levels of aerobic exercise decrease the risk of atrial fibrillation, excessive exercise especially as we age causes an increased risk.
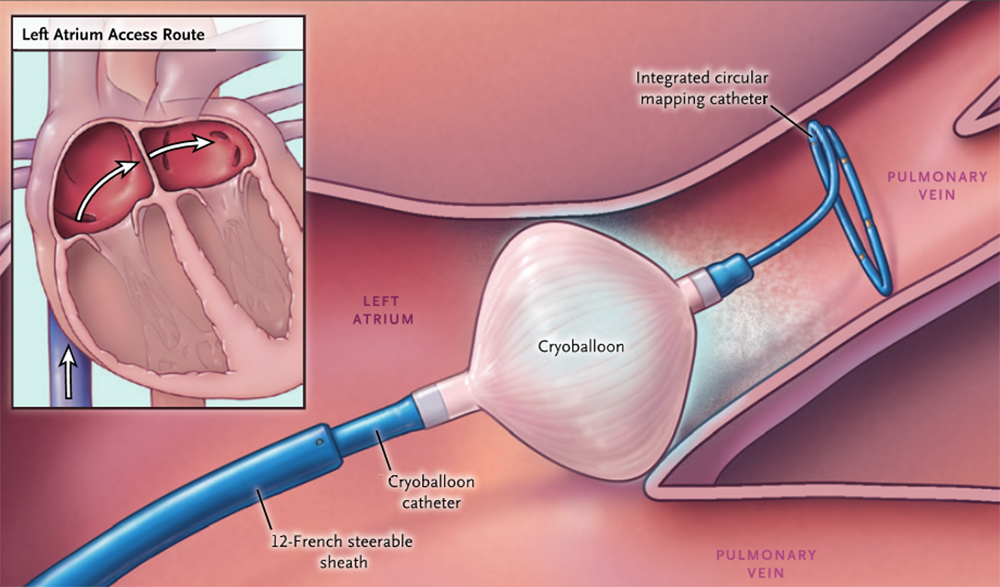
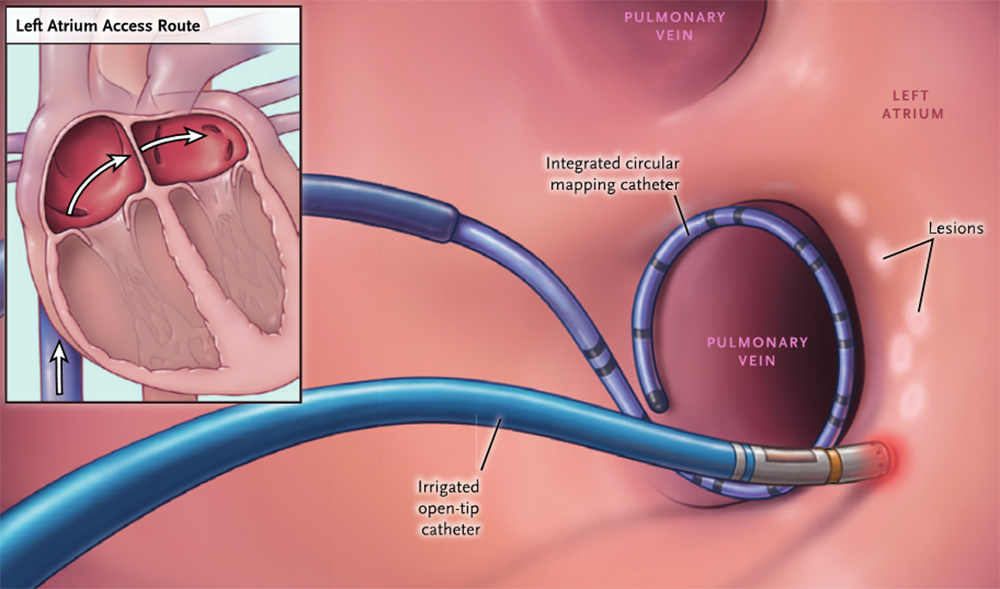
CATHETER ABLATIONS
If there is no improvement with medications, usually an ablation is recommended. Sometimes ablation is the first treatment for certain patients.
The procedure is performed by passing a into the heart through one of the blood vessels. During an ablation we aim to create a line of electrical block around the pulmonary veins (the main source of atrial fibrillation). There are two main modalities outlined below, radiofrequency and cryotherapy.